Esplenomegalia e icterícia en canales de cerdo
El estudio histopatológico de las muestras de hígado y bazo revela que el hígado no presenta lesiones significativas, los cambios del bazo se deben a extensas áreas hemorrágicas. Se descartan lesiones de tipo inflamatorio-necróticas.
No se puede determinar la causa de estas hemorragias, pero muy probablemente se deben a una torsión esplénica o a traumatismos. La causa del ictericia y si tiene relación con la torsión esplénica es incierta. Una posibilidad sería que la degradación de los eritrocitos extravasados hubiera producido la ictericia, se trataría entonces de una ictericia prehepàtica por hemólisis.
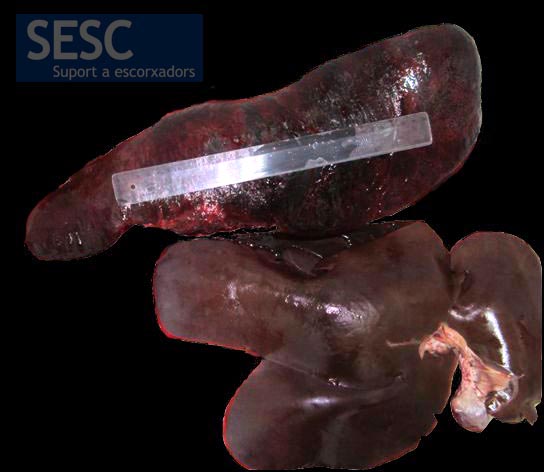
Aumento del tamaño del bazo (50 cm x 20 cm) con cambios de coloración en la superficie. El hígado no presentaba alteraciones.
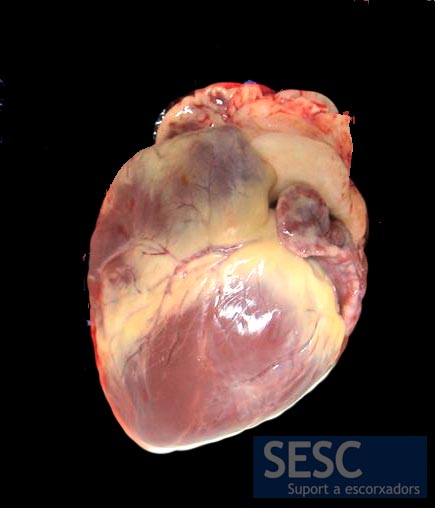
Los cambios de coloración amarillenta (ictericia) eran evidentes en el tejido adiposo pericárdico así como a la esclera, los endotelios y la pelvis renal.
.


10 comment(s)
Hello, I’m André Van Roy, a Belgian veterenary meat inspector.I ‘ll rephrase my question of january 2023. In your view, is the meat from these carcasses harmfull to the consumers health?
Excuse us for the delay in answering, André, and thank you for reading our blog. According to Regulation UE 2019/627 article 45, letter o) carcasses with yellow discolouration (jaundice) should be condemned (indicates pathological or organoleptic changes, in particular a pronounced sexual odour or insufficient bleeding (except for wild game)). But it is true that in cases where an hepatic jaundice can be ruled out, and there’s a splenic torsion (suggestic pre-hepatic jaundice) and the coloration is mild, the literature suggests to wait and see if the coloration fades in time, to avoid condemnation. Ultimately the inspector’s criteria gathering all the information of the case (other lesions, additional inspections, etc) will determine whether or not that particular carcass has to be condemned. We do have observed an increasing trend of pig carcass condemnation due to jaundice over the last 10 years, with conspicuous seasonal peaks in the summer months.
Over here in Belgium we see this verry often, mostly the carcasses get condemned for peritonitis.
How do you judge these carcassses in your country?
Should a carcas with prehapatic icterus due to torsion of the spleen ( and mild jaundice ) be condemned?
Buenas noches he visto en necropsias en cerdas gestantes, aumentos de volumen (abscesos) en bazo que destruyen tejido esplenico, de aspecto neoplasico. Que agentes etiologicos pueden estar involucrados?
I also have similar cases. Which are visually very similar. In the present case, but I would rule out torsion and injury, because even two cases in one group of animals it is unlikely.
There are a number of pathogens that may cause jaundice in pigs, being the most usual one Mycoplasma (Eperythrozoon) suis. In that particular case, M. suis was not investigated, since just two pigs from the batch showed jaundice. Moreover, jaundice is usually linked to hepatic damage and/or hemolysis as the most common generic causes, but no presumable relationship with spleen necrosis has been described as far as we know. In pigs, to our knowledge, no protozoan parasites are known to cause jaundice.
Comment form LinkedIn:
I don’t know about the pig . How about the protozoal diseases?
Thank to your slides.
SESC’s pathologists answer is:
There are a number of pathogens that may cause jaundice in pigs, being the most usual one Mycoplasma (Eperythrozoon) suis. In that particular case, M. suis was not investigated, since just two pigs from the batch showed jaundice. Moreover, jaundice is usually linked to hepatic damage and/or hemolysis as the most common generic causes, but no presumable relationship with spleen necrosis has been described as far as we know. In pigs, to our knowledge, no protozoan parasites are known to cause jaundice.
Comment from LinkedIn:
Did you check these animals for Hep E virus?
Our pathologists answer:
We have no information about the status of infection with HEV in this pig. From our previous studies with HEV, many pigs in a herd become infected, in a totally subclinical way, even with no demonstrable lesions in the liver. The only way to rule out a HEV infection would be by PCR in liver tissue or in bile. We are not aware of a relationship between HEV and spleen lesions.
For further reference:
de Deus, N., Casas, M., Peralta, B., Nofrarias, M., Pina, S., Martin, M., Segales, J., 2008, Hepatitis E virus infection dynamics and organic distribution in naturally infected pigs in a farrow-to-finish farm. Vet Microbiol 132, 19-28.
de Deus, N., Seminati, C., Pina, S., Mateu, E., Martin, M., Segales, J., 2007, Detection of hepatitis E virus in liver, mesenteric lymph node, serum, bile and faeces of naturally infected pigs affected by different pathological conditions. Vet Microbiol 119, 105-114.
Comment from LinkedIn:
Nice pictures. This incidental finding did me remember an other spleen problem the spleen atrophy. Is the spleenmegaly resolvebel ( ?) and ending in an atrophy?
Our pathologists answer:
Thanks for your comment. After a spleen torsion, the probable evolution of the lesion would be to a ischemic necrosis of the spleen, and sequester formation. The spleen would not be functional anymore. In strict sense it would not be appropriate to speak about atrophy, as the organ is not involved in a progressive reduction of the tissular component.